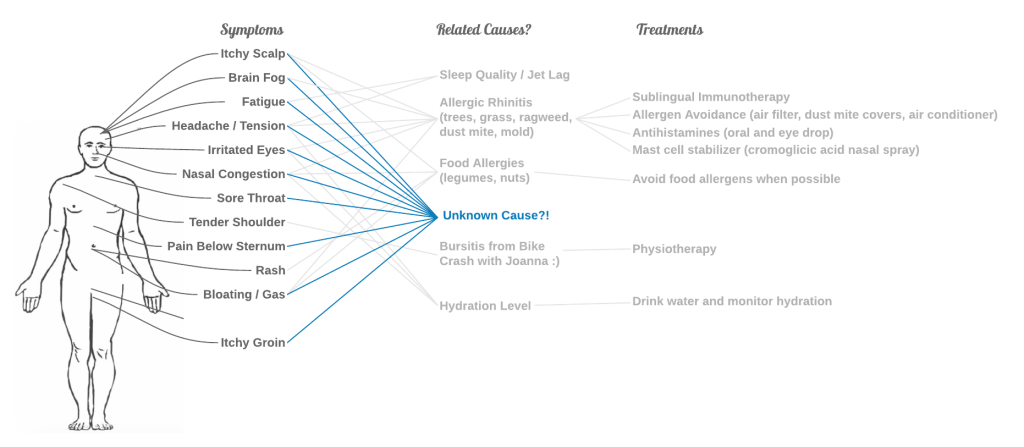
On May 25th this year, Joanna and I went on a biking Meetup through the beautiful forests in Brandenburg. We stopped for a drink at Kuddel’s, a small, leafy beer garden by the Dahme river. I left with a mild feeling of brain fog, stuffy nose, and itchy eyes. I thought that this must be my tree and grass pollen allergies acting up. Berlin was in peak allergy season, and I had just biked 40km outside, all day.
Later that day, our wonderful next door neighbor invited us over for her 50th birthday. One of her old housemates from college made Joanna and I an Old Fashioned. Soon, I started feeling deeply exhausted and sleepy. Every person in the room made me feel anxious. My mind slowed to half speed and I found it hard to follow conversations. The turbinates in my nose expanded and each breath took a bit more work. My eyelids grew swollen and sticky. My stomach and scalp itched strongly.
At first, I thought this might be a delayed allergic reaction to biking outside all day. Over the next few weeks, sensations like these happened regularly. They came at random and made themselves at home for a few hours or a day or two.
Joanna and I doubled down on allergy controls. I had already adapted most of my US allergy avoidance and treatment routine to Berlin. On the flight over, I’d carried a 6-month supply of allergy medications. I had two bottles of my sublingual immunotherapy drops. We packed our dust-mite proof mattress and pillow covers. One of our first purchases in Berlin was a room air filter. In the warm summer, we kept the windows closed and used A/C, which nobody does in Germany. I knew the pollen calendar by heart and had found reliable local pollen forecasts.
Soon, I sensed this wasn’t the same old allergies. Even when I was in my pristine, allergy-controlled bubble at home, the symptoms came. They came quickly, often after a meal, in waves and patterns that felt unfamiliar. Half the days of the week, I had too much brain fog to concentrate on my side projects and learning German. What could possibly cause all these reactions, all at once?
I felt like I couldn’t trust my body. Like the early days in my allergy journey 15 years ago, I felt frustration and subtle hesitation. I could not commit to doing things when my body might shut down on a whim. This was not normal and I was not ready to accept continuing like this. I had to try something else.
The Elimination Diet
In early June, I called my allergist in San Francisco to talk about the new mystery symptoms. He recommended trying an elimination diet.
I looked online for resources on how to run such a diet. After some searching, I found Michael Ruscio’s book “Healthy Gut, Healthy You.” In a sea of pseudoscience gut health resources, this book at least tried to be evidence-based. It was honest about what’s backed by research or not. For example, Ruscio used IgG food sensitivity tests in his practice, but stopped after realizing they produced more noise than signal.
Ruscio’s principles for running a diet experiment seemed thoughtful and lined up with my allergist’s recommendations. These are some key parts I gleaned from the book:
- Reset
Start with a very simple diet to reset the digestive system (e.g. liquid fast with bone broth or lemonade) - Organize by food group
Plan around adding or removing categories of food. Choose groups in an order that might reveal the most. For example, Ruscio recommended starting with a Paleo diet and if that didn’t help much, moving to an autoimmune Paleo diet (minus common allergens like dairy, gluten, legumes, eggs) - Personalization
Each person has different dietary needs, based on personal factors and ancestral history. No diet is universally healthy. For example, if you ascribe to eating like your hunter-gatherer ancestors, they differed wildly in carbohydrate consumption depending on where they lived. - Wait and see
Give each major change in diet 2-3 weeks and track symptoms. It takes time for the gut and body to respond to changes. - Avoid angst
Don’t fret about sticking 100% to a diet. Going off plan once in a while won’t make a big difference. Hiding in a hole and avoiding friends is worse.
Data to the Rescue!
For those who’ve worked with me, you know I’m a bit of a data nerd. I wanted a food diary that could help me and my allergist understand my symptoms.
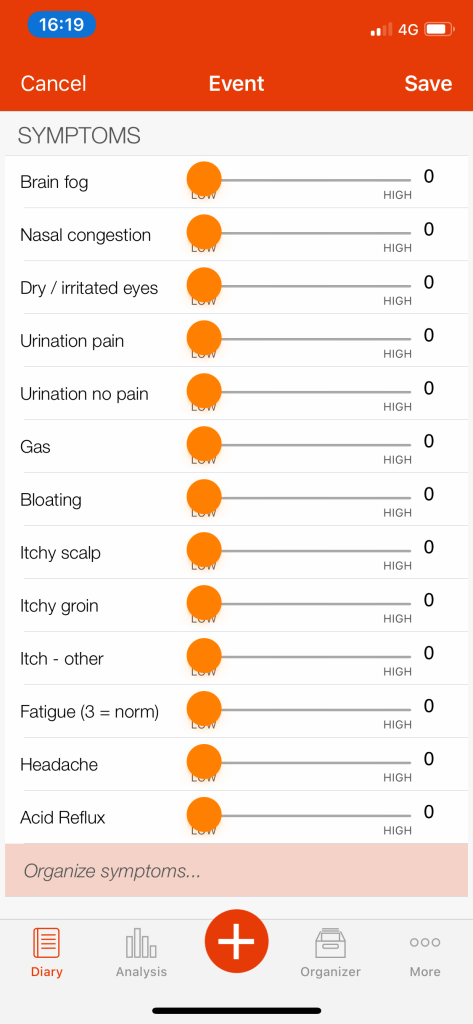
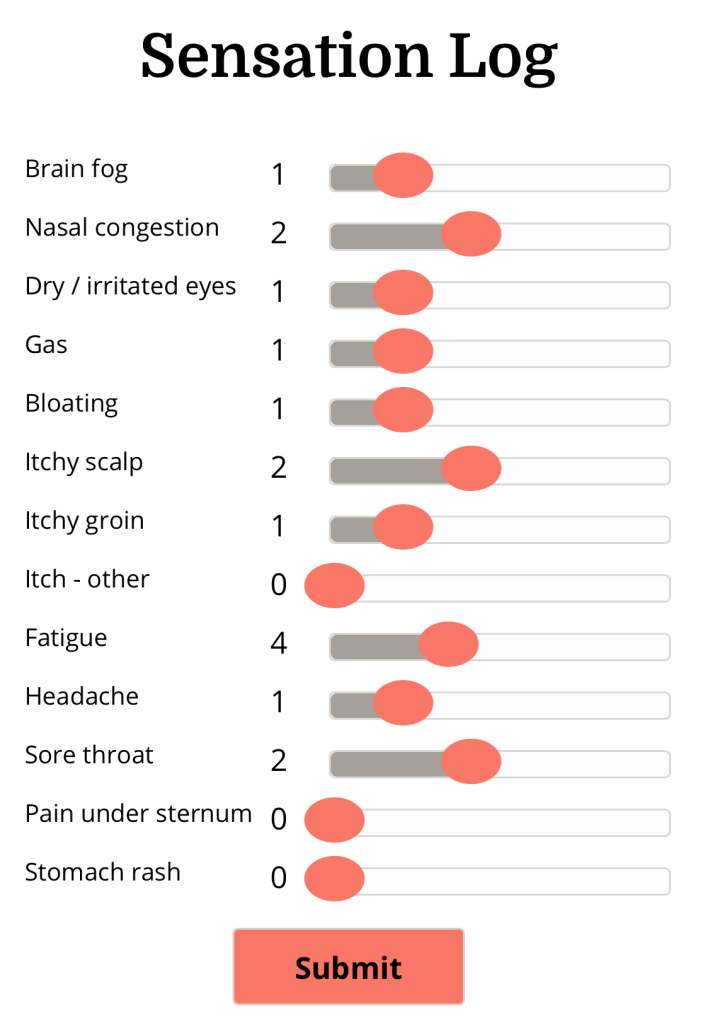
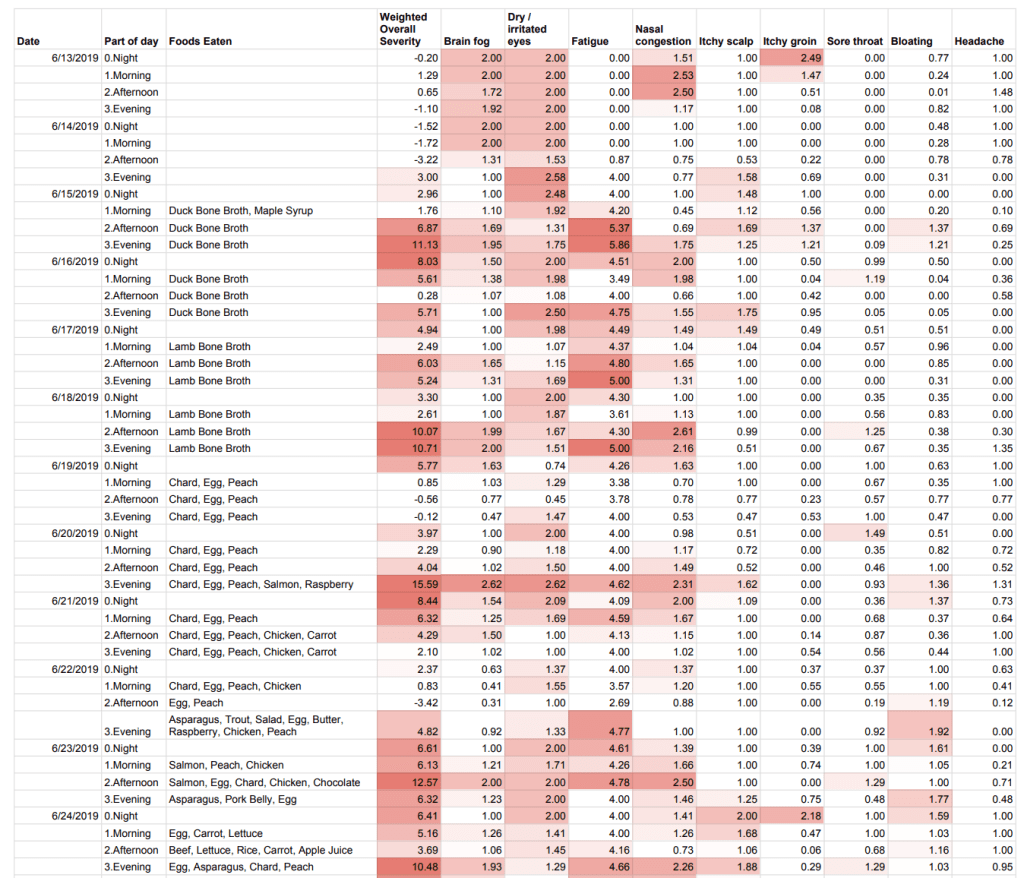
I hoped to understand correlations between my sensations and triggers. To do this, I wanted to know how my sensations varied over time, with subjective but comparable measurements. I decided on a list of sensations to track and what scales to use (e.g. Mankowski pain scale, Bristol poop scale). I also wanted to track potential triggers, especially foods eaten.
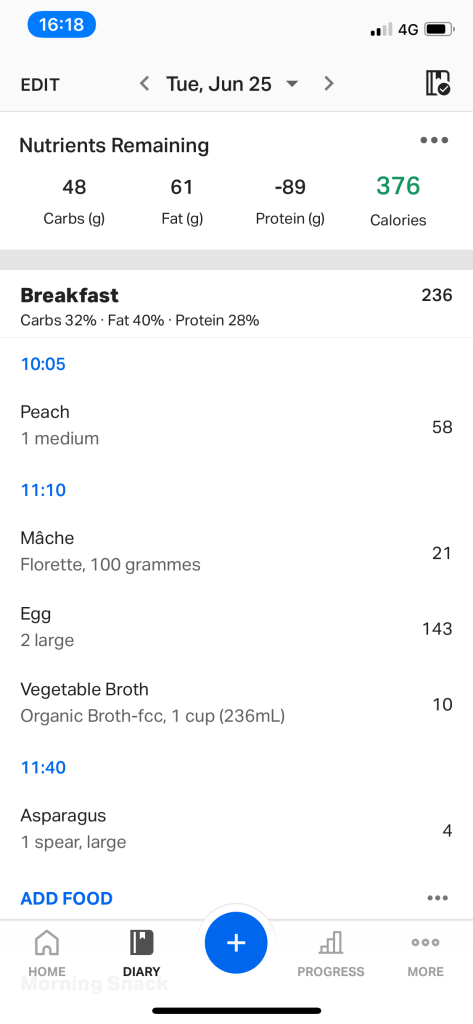
For those who’ve worked with me, you also know that I’m a lazy engineer (the best kind). The less work I need to do to get things done, the better. So before the diet, I looked for an app that did what I needed. I hoped there might be a single app, and mySymptoms came close. But while it had a good symptom tracking UI, its food tracking and correlations were meaningless. So I added MyFitnessPal in for food tracking and resigned myself to merging and analyzing the data on my own.

Running Experiments
Following Ruscio’s guidelines, I started with 4 days of liquid-only fast to cleanse the digestive system. Then 3 weeks of Autoimmune Paleo, slowly adding 2-3 foods every couple of days. I skipped Ruscio’s recommendation to start with Paleo, because I already knew I had nut and legume allergies and issues with dairy.
The video below shows meals I ate over time, with a few new foods added every day or two. If the foods seemed safe, I would keep eating them. The first few days were all chard and eggs, but soon chicken, carrots, and many more foods joined the safe list. We cooked chard in so many different ways! I also ran into foods that were often bad, like strawberries, raspberries, chocolate, salmon, and aged cheeses.
I worried briefly about how I would react to such a limited diet. But trips to the grocery store felt freeing — when I could only eat a few things, I breezed through the aisles and didn’t need to make choices.
Better Tools and Reports
After a few weeks, I understood more about what I wanted in my food diary. MyFitnessPal took too much work and I didn’t need the detailed calorie counts. Instead, I started entering foods eaten directly into my spreadsheet. Also, the work to transfer data from mySymptoms was annoying, so I built my own web page. It logged sensations into the spreadsheet and updated reports.
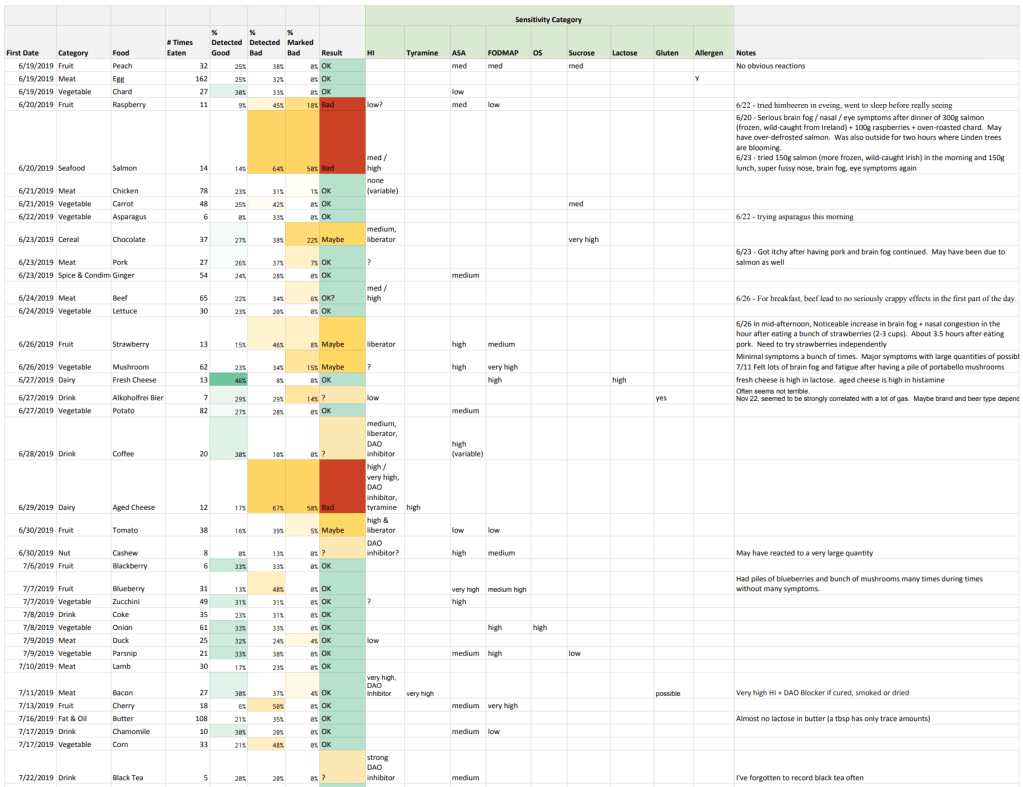
I made reports to answer key questions. One was a daily food diary to see how sensations varied, every 6 hour period, with foods eaten. Another summarized foods from the daily diary as likely good or bad and mapped each food to sensitivity categories from a Baliza Food Intolerance app. This made it possible to tie sensations to foods, and foods to types of sensitivity.
What I Learned So Far
By mid-July, I understood much more about my body. Symptoms happened in three different ways: food allergens like nuts triggered mainly itching, dairy triggered bloating and gas, and the “bad” foods triggered almost all of the sensations. Symptoms tended to come an hour or two after eating and lasted for half a day to a day. From the food sensitivity report, I started guessing that I might have histamine issues. Joanna started joking that I’m a “sensitive man.”
Histamine plays an important role in immune response, gut regulation, and as a neurotransmitter. These are normally good things. Yet, it’s possible for the body to absorb too much histamine into the bloodstream. It can also have too little Diamine Oxidase (DAO), the enzyme that breaks down and regulates histamine.
Many foods contain histamine that gets absorbed in the gut. Many foods develop histamine when they decay. So not only does the kind of food matter, but also how it was handled. For example, when ground meat is not kept cold enough, it has more surface area and spoils quickly. Most fermented or aged foods develop high levels of histamine (e.g. soy sauce, aged cheese, beer). A few items like lemon juice and chocolate liberate histamines, causing the body to release more histamine. The list of foods is quite long (see this Swiss interest group’s food compatibility list)
Having a plausible story only raised more questions. Was I really histamine intolerant, or could it be something else? What caused this? What could I do about it? Would I ever eat dim sum or fondue again?
I needed more expert help to interpret and act on what I was learning. On July 24th, I started reviewing my symptoms with doctors. That journey through the American and German medical systems is a story for another time.
In parallel, I continued experimenting and keeping a food diary. I tested more histamine-rich foods, but I also started systematically avoiding them. I wanted to try and live life as best as I could.

Leave a comment